Peer Review in Radiation Oncology: Where Does the Middle East, North Africa, and Turkiye Region Stand?
Abstract
Purpose
This study aims to assess the status of radiation oncology peer review procedures across the Middle East, North Africa, and Turkiye (MENAT) region.
Methods
A cross-sectional electronic survey was conducted among radiotherapy centers in the MENAT region in March 2024. It assessed peer review practices, departmental demographics, perceived importance of peer review, and potential barriers.
Results
Data from 177 radiation oncology centers revealed varying peer review implementation across the MENAT region. Egypt had the highest participation (16.4%) among all responders. Most centers (31%) treated 500-1,000 cases annually. The majority (77.4%) implemented peer review, with varying levels between countries and across different centers. Advanced radiotherapy techniques significantly correlated with implementation of peer review (P < .05).
Peer review meetings were mostly scheduled on a weekly basis (46%) and organized by radiation oncologists (84.7%). Target volume contouring (89%) and radiotherapy prescription (82%) were frequently peer-reviewed. Respondents with peer review at their institutions significantly valued peer review for education, adherence to guidelines, improving planning protocols, and reducing variation in practice institutions without peer review (P < .05). The most frequently reported barriers to peer review were having a high number of patients (56%) and shortage of time (54%).
Conclusion
Peer review is essential for improving the quality of practice in radiation oncology. Despite some discrepancies, numerous obstacles, and challenges in implementation, it is instrumental in the improvement of patient care in most centers throughout the region. Raising awareness among radiation oncologists about the importance of peer review is paramount to lead to better outcomes.
Introduction
Peer review plays a crucial role in ensuring the quality, safety, and efficacy of medical practices, and nowhere is this more evident than in radiation oncology. It is defined by the Royal College of Radiologists as a formal review of the delineated contours by another site-specific oncologist, undertaken alongside a review of dose and fractionation.
Radiotherapy plans may require modifications in target volume delineation, dose/fractionation schedules, planning objectives, organs-at-risk dose constraints, and the intention of treatment to improve the quality of the delivered treatment.
Despite its recognized importance, the implementation and status of peer review practices can vary significantly across different regions and health care settings, especially in underprovided areas such as the Middle East, North Africa, and Turkiye (MENAT). This is especially important when considering how cancer represents a disproportionate burden in low- and middle-income countries (LMICs), many of which lie in this region. The health care systems in many of these countries also face several challenges, such as inadequate workforce and infrastructure to provide access to radiotherapy.
As of March 2024, and according to the International Atomic Energy Agency (IAEA), 20 countries in the MENAT region have access to radiotherapy, with 462 centers. A disproportionate number of these centers are found in selected countries; most are found in Turkiye, which contains 142 centers, followed by Iran with 84 centers and Egypt with 75 centers.
This study evaluates the current peer review landscape in radiation oncology within this geographical context. Not only does this contribute to the global discourse on quality assurance, but it also provides valuable insights for improving patient care in these diverse health care settings.
Methods
The study protocol received the required approval from the Institutional Review Board (IRB) at the King Hussein Cancer Center (IRB number: 23 KHCC 165). Information regarding radiotherapy centers was gathered from IAEA’s Directory of Radiotherapy Centers. A cross-sectional electronic survey of peer review practices in the MENAT region was distributed to potential participants via email. Cancer centers without radiotherapy services and those outside the MENAT region were excluded. The research team adapted and subsequently piloted a self-administered questionnaire, initially developed by Rubagumya et al. and it was revised on the basis of respondents’ feedback. The survey was administered in English as it is a language in which the health care workers of the region are proficient. Only one representative per cancer center was allowed to complete the survey; however, they were encouraged to consult their multidisciplinary radiation oncology team.
The main topics of the survey included departmental demographics, the current state of peer review at the center, and how it is conducted, scheduled, and organized. It also covered the types of cases reviewed, participation by different disciplines, the use of advanced technology, and obstacles to conducting peer reviews.
Survey data were imported into Statistical Package for the Social Sciences, version 27.0 for Windows (IBM, Armonk, NY). The analysis was primarily descriptive, including frequencies and percentages for categorical data. Chi-square tests were used to compare the volume and complexity of technology between centers that did and did not report the use of peer review. By contrast, t-tests were used to compare the perceived importance of the peer review process between centers that did and did not report the use of peer review. P < .05 was considered statistically significant.
Results
Characteristics and Distribution of Radiation Oncology Centers in the MENAT Region
The survey gathered data from 177 radiation oncology centers across the MENAT (38%). Egypt had the highest frequency of participation (n = 29, 16.4%), followed by Iran with 21 centers (11.9%) and Turkiye with 19 centers (10.7%).
Regarding the number of new patients treated per year per center, most fall within the range of 500-1,000 patients, accounting for 31.1%, whereas centers treating 1,000-2,000 patients annually make up 29.9%. In terms of available equipment and techniques, three-dimensional (3D) computed tomography (CT) simulation is the most prevalent (91.5%), followed by four-dimensional (4D) CT (40.7%), with breath-hold methods being used in 43.5% of the centers. Cyberknife and Gamma Knife are available in only a few centers, at 1.7% and 1.1%, respectively. (Table 1)
Treatment planning techniques show a range of options, with 92.7% offering 3D conformal radiation therapy and 79.1% providing intensity-modulated radiation therapy (IMRT). As for verification imaging modalities, megavoltage is the most commonly available (76.3%), followed by cone beam CT (66.1% (Table 1)). Overall, 77.4% of the participating centers have implemented peer review practices, with varying rates across countries: 72.4% of Egyptian centers, 89.5% of Turkish centers, and 100% of Saudi centers. Meanwhile, only 33.3% of Iranian centers implemented peer review practices at their institutions.
| Variable | No. (%) |
|---|---|
| Country | |
| Algeria | 7 (4) |
| Bahrain | 1 (0.6) |
| Egypt | 29 (16.4) |
| Iran | 21 (11.9) |
| Iraq | 9 (5.1) |
| Jordan | 7 (4) |
| Kuwait | 2 (1.1) |
| Lebanon | 8 (4.5) |
| Libya | 4 (2.3) |
| Morocco | 16 (9) |
| Oman | 2 (1.1) |
| Pakistan | 15 (8.5) |
| Palestine | 1 (0.6) |
| Qatar | 1 (0.6) |
| Saudi Arabia | 16 (9) |
| Sudan | 3 (1.7) |
| Syria | 2 (1.1) |
| Tunisia | 5 (2.8) |
| Turkiye | 19 (10.7) |
| United Arab Emirates | 8 (4.5) |
| Yemen | 1 (0.6) |
| Total | 177 (100) |
| No. of new patients treated per year per center | |
| <500 | 32 (18.1) |
| 500-1,000 | 55 (31) |
| 1,000-2,000 | 53 (29.9) |
| 2,000-3,000 | 21 (11.9) |
| 3,000-4,000 | 7 (4) |
| >4,000 | 9 (5.1) |
| Total | 177 (100) |
| Available equipment and techniques | |
| 4D CT | 72 (40.7) |
| 3D CT | 162 (91.5) |
| Abdominal compression | 60 (33.9) |
| Breath-hold methods | 77 (43.5) |
| Conventional fluoroscopy | 68 (38.4) |
| Cyberknife | 3 (1.7) |
| Gamma knife | 2 (1.1) |
| Available treatment planning techniques | |
| 2D or clinical mark-up treatment planning | 59 (33.3) |
| 3D conformal radiation therapy | 164 (92.7) |
| Intensity-modulated radiation therapy | 140 (79.1) |
| Volumetric modulated arc therapy | 124 (70.1) |
| Stereotactic body radiotherapy | 94 (53.1) |
| Stereotactic radiosurgery | 81 (45.8) |
| Total body irradiation | 42 (23.7) |
| Total skin irradiation | 17 (9.6) |
| Adaptive radiotherapy | 58 (32.8) |
| Available imaging modalities | |
| Megavoltage | 135 (76.3) |
| Kilovoltage | 74 (41.8) |
| Cone beam CT | 117 (66.1) |
Associations Between Available Techniques and the Presence of Peer Review
Associations between available techniques and the presence of peer review within the participating centers are listed in Table 2 . There was a significant association between the availability of 4D CT (P = .001), IMRT (P = .04), volumetric modulated arc therapy (VMAT; P < .001), stereotactic radiosurgery (SRS; P = .03), and total body irradiation (TBI; P = .006) and the presence of peer review practices, whereas there was no association with the other listed techniques.
| Available Technique | Presence of Peer Review, Yes (No. %) | Presence of Peer Review, No (No. %) | P |
|---|---|---|---|
| 4D CT | 65 (47.4) | 7 (17.5) | .001 |
| 3D CT | 126 (92) | 36 (90) | .694 |
| Abdominal compression | 50 (36.5) | 10 (25) | .19 |
| Breath-hold methods | 64 (46.7) | 13 (32.5) | .147 |
| 2D or clinical mark-up treatment planning | 43 (31.4) | 16 (40) | .309 |
| 3D conformal radiation therapy | 126 (92) | 38 (95) | .735 |
| IMRT | 113 (82.5) | 27 (67.5) | .04 |
| VMAT | 105 (76.6) | 19 (47.5) | <.001 |
| SBRT | 78 (56.9) | 16 (40) | .072 |
| SRS | 69 (50.4) | 12 (30) | .03 |
| TBI | 39 (28.5) | 3 (7.5) | .006 |
| TSI | 15 (10.9) | 2 (5) | .367 |
| Adaptive radiotherapy | 50 (36.5) | 8 (20) | .057 |
Peer Review Structures and Planning
Peer review rounds are predominantly timetabled into the job (68.6%) rather than being ad hoc when needed (31.4%). The frequency of peer review meetings varies, with weekly sessions being the most common (46%), followed by twice weekly (18%). Most centers (71%) review curative and palliative patients during peer review sessions. The sessions are most commonly organized by the radiation oncologist (84.7%). Radiation oncologists are almost always present at these meetings (96.4%). The time needed for one patient review typically ranges from 5 to 10 minutes (53%). Sessions usually last between 30 and 60 minutes (49%) and are often conducted prospectively before commencing treatment (49%). Face-to-face sessions in the local institution are the most prevalent mode of conducting peer review (80%; Data Supplement, Table S2).
Outcomes of the Peer Review Process
Table 3 presents the outcomes of the peer review process. Regarding the proportion of plans peer-reviewed, a significant portion of curative plans are reviewed, with 30% of centers reporting an 80%-100% review rate, whereas for palliative plans, a lower percentage of centers (10%) achieves the same level of review. Target volume contouring is the most frequently peer-reviewed part of the treatment plan (89%), followed by radiation dose prescription (82%) and radiotherapy planning dose distribution (79%). Recommendations resulting from peer review are often recorded in the patient’s chart (76%). After peer review, many plans were modified, with 74% suggesting minor changes and 50% undergoing major changes, whereas only a small percentage (4.4%) remains unchanged (Fig 1).
Figure 2 presents the perceived importance of radiation oncology peer review across various aspects. On a scale from 1 to 10, with higher values indicating greater importance, the mean scores indicate that respondents highly value peer review as a platform for continuous medical education for radiation oncologists (mean, 8.9; standard deviation [SD], 1.7) and as an educational opportunity for trainees (mean, 8.93; SD, 1.7). In addition, peer review is perceived as crucial for assessing conformity to clinical practice guidelines (mean, 9.03; SD, 1.5), allowing improvement of the multidisciplinary team process (mean, 8.95; SD, 1.6), and enhancing planning protocols (mean, 8.94; SD, 1.6). Furthermore, respondents acknowledge the role of peer review in reducing variation in practice (mean, 8.72; SD, 1.7). Overall, the perceived importance of radiation oncology peer review is high, with an overall mean score of 8.99, SD 1.4, underscoring its significant role in ensuring quality and consistency in patient care and professional development.
| Variable | Frequency | Percentage of Centers With Peer Review |
|---|---|---|
| Proportion of curative plans peer-reviewed | ||
| < 20% | 16 | 12 |
| 20%-49% | 22 | 16 |
| 50%-79% | 45 | 33 |
| 80%-100% | 41 | 30 |
| Not sure | 13 | 9 |
| Proportion of palliative plans peer-reviewed | ||
| < 20% | 58 | 42 |
| 20%-49% | 42 | 31 |
| 50%-79% | 7 | 5 |
| 80%-100% | 14 | 10 |
| Not sure | 16 | 12 |
| Part of the plan that is peer-reviewed | ||
| Target volume contouring | 122 | 89 |
| Dosimetry | 108 | 79 |
| Prescription | 112 | 82 |
| Indication | 7 | 5 |
| Follow-up plan after peer review | ||
| Recommendations recorded in the chart | 104 | 76 |
| Established process for follow-up | 44 | 32 |
| Radiation oncologists compelled to adhere | 38 | 28 |
| Attendance list recorded | 33 | 24 |
| Change to radiation therapy plan after peer review | ||
| Minor change | 101 | 74 |
| Major change | 68 | 50 |
| No change | 6 | 4 |
Importance of the Peer Review Process
Table 4 compares the perceived importance of the peer review process between centers with and without peer review mechanisms. Centers with peer review generally rate the process as more highly important in various aspects than those without. Centers with peer review perceive it as a significantly more valuable educational opportunity for trainees (mean, 9.11 v 8.3; P = 0.015) and to assess conformity to clinical practice guidelines (mean, 9.18 v 8.5; P = 0.011). In addition, peer-reviewed centers see peer review as more critical for improving planning protocols (mean, 9.09 v 8.43; P = 0.018) and reducing variation in practice (mean, 8.86 v 8.25; P = 0.046). While the overall perceived importance of peer review does not reach statistical significance (mean, 9.09 v 8.63; P = 0.070), the trend indicates a generally higher regard for peer review in centers that have implemented it.
| Peer Review Objective | P | ||||
|---|---|---|---|---|---|
| Presence of Peer Review | No. | Mean | Standard Deviation | ||
| As a platform for continuous medical education for radiation oncologists | Yes | 137 | 9.00 | 1.613 | .15 |
| No | 40 | 8.55 | 2.099 | ||
| As an educational opportunity for trainees | Yes | 137 | 9.11 | 1.644 | .01 |
| No | 40 | 8.30 | 2.409 | ||
| To assess conformity to clinical practice guidelines | Yes | 137 | 9.18 | 1.324 | .01 |
| No | 40 | 8.50 | 1.935 | ||
| To allow improvement of the multidisciplinary team process | Yes | 137 | 9.04 | 1.401 | .17 |
| No | 40 | 8.65 | 2.007 | ||
| To improve planning protocols | Yes | 137 | 9.09 | 1.348 | .02 |
| No | 40 | 8.43 | 2.074 | ||
| To reduce variation in practice | Yes | 137 | 8.86 | 1.506 | .04 |
| No | 40 | 8.25 | 2.227 | ||
| Overall perceived importance | Yes | 137 | 9.09 | 1.288 | .07 |
| No | 40 | 8.63 | 1.849 | ||
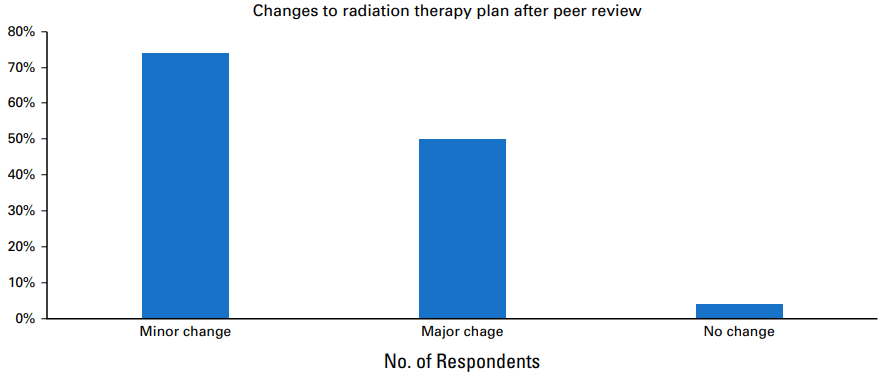
Figure 1 The distribution of radiation therapy plans on the basis of changes required after peer review. Plans were categorized into three groups: those requiring minor changes, those requiring major changes, and those requiring no changes. Data are presented as percentages.
Barriers to Initiating Peer Review
Table 5 outlines the perceived barriers to initiating or sustaining peer review. The most cited barrier is the high number of patients, with 56% of respondents indicating this issue, followed by shortage of time (54%) and being shortstaffed (46%).
| Barrier | No. (%) |
|---|---|
| High number of patients | 99 (56) |
| Shortage of time | 95 (54) |
| Shortage of staff | 82 (46) |
| Lack of policy | 62 (35) |
| Inadequate communication among radiotherapy professionals | 55 (31) |
| No interest among colleagues | 45 (25) |
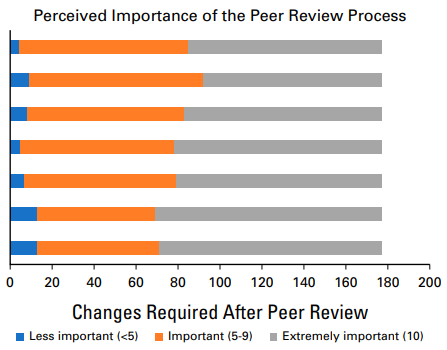
The perceived importance of the radiation oncology peer review process among survey respondents. Importance ratings were collected using a Likert scale ranging from 1 (not important) to 10 (extremely important). Respondents who rated the process below 5 indicated it as less important, whereas ratings between 5 and 9 denote varying degrees of importance. A score of 10 indicates that the process was deemed extremely important. Data represent responses from 177 participants.
Discussion
Peer review is essential for quality assurance in radiation oncology, preventing serious harm or poor outcomes via addressing subjective treatment decisions. Our survey found that 77.4% of institutions practiced peer review, similar to those in North America and sub-Saharan Africa. Most participants reviewed target volume contours (89%), dose distribution (79%), prescription (82%), and indication (5%), consistent with other regions. In the literature, common issues discussed and modified include dose and fractionation, normal tissue exposure, target volume coverage, and treatment techniques.
While 50% of patients with cancer globally need radiotherapy, access is highly heterogeneous. Worldwide, 31% of LMICs lack any radiotherapy facilities. As of March 2024, the IAEA reports that 20 MENAT countries have 462 centers for over 578 million people. Establishing radiotherapy programs requires substantial investment, which is challenging for LMICs with other public health priorities. Centers in the MENAT typically treat 500-1,000 patients annually, similar to sub-Saharan Africa.
While most survey respondents reported access to certain techniques, significant gaps remain in accessing more advanced techniques such as SRS (45.8%), 4D CT (40.7%), TBI (23.7%), TSI (9.6%), Cyberknife (1.7%), and Gamma Knife (1.1%). These numbers are comparable globally. For instance, in Australia and New Zealand, IMRT was used by 91.3% of centers, whereas VMAT was used by only 56%. Meanwhile, in the United Kingdom, 74% of centers use VMAT techniques. Our study identified significant associations between the availability of 4D CT (P = .001), IMRT (P = .04), VMAT (P < .001), SRS (P = .03), and TBI (P = .006) and the implementation of peer review practices. These advanced techniques highlight the growing importance of peer review.
In 68.6% of centers that participated in the survey, peer review practices are scheduled regularly, whereas they are used on an as-needed basis in 31.4% of centers. Providing protected time for peer review practices is preferred over ad hoc, ensuring a more systematic and structured approach for such a critical quality assurance measure. A study from North America demonstrated that providing structured time for and monitoring attendance of peer review sessions resulted in increased participation by senior faculty as well.
Interestingly, respondents reported that curative and palliative plans were reviewed most of the time (71%). Meanwhile, in Canada, only 13% of all plans were peer-reviewed; among those, 85% was curative. Radiation oncologists were typically present at peer review sessions with medical physicists, residents, radiation therapy technicians, and various other allied health professionals, similar to reports from other regions. The diversity of participants reflects the collaborative nature of treatment planning and delivery. The combined experience of the planner and physician determines the best plan and ensures a multidisciplinary approach to reviewing and treating patients.
Most respondents held weekly peer review sessions lasting 30-60 minutes, with patients reviewed in 5-10 minutes each. By contrast, the North American study reported shorter sessions under 2 hours per week, reviewing patients in 2.7 minutes each. Most respondents also reported that their peer reviews were predominantly prospective or a mix of prospective and retrospective. The American Society for Radiation Oncology (ASTRO) recommends prospective peer review as discussion with patients whose therapy has already been initiated is less useful. Prospective reviews help prevent errors, whereas retrospective reviews may occasionally identify errors in cases that went awry or when unexpected toxicities or poor outcomes occurred.
While 76% recorded recommendations in patients’ charts, only 32% had a formal follow-up process, and adherence to recommendations was required in just 28% of patients, contrary to ASTRO guidelines advocating for individual tracking of peer review outcomes. In addition, attendance was recorded in only 76% of sessions conducted at our respondents’ centers. Tracking attendance is of particular importance as, in the aforementioned North American study, attending physicians were present 69% of the time in departments with documented attendance, versus only 29% of the time in centers without.
As for changes to the radiotherapy plan after peer review, our respondents reported high percentages of alterations; 74% reported minor changes, whereas 50% reported major changes. These numbers are notably higher than those reported from centers in North America, where peer review led to changes in care around 10% of the time. They also differed from Canadian data, where minor changes occurred in 6% of patients, whereas major changes occurred in only 1% of patients. The Canadian study found that more experienced radiation oncologists were recommended fewer modifications. Therefore, as newer radiotherapy centers gain experience, the number of suggested alterations is expected to decrease.
When respondents were asked about the perceived importance of the peer review process, most viewed all aspects as extremely important, which is to be expected, given the existing data on the necessity of peer review. Interestingly, centers with peer review perceive it as a more valuable educational opportunity for trainees and a means to assess conformity to clinical practice guidelines. While centers without peer review may initially underestimate its significance, they should not overlook its importance as a commitment to excellence, continuous learning, and the delivery of evidence-based care.
Respondents reported several barriers to peer review, such as too many patients, limited time, and insufficient staff. Despite these challenges, implementation remains necessary, and ASTRO recommendations offer many solutions. Leadership can expand peer review by dedicating time, creating regional guidelines, and mandating institutional implementation. Virtual peer review meetings, used by some centers, help smaller centers in places like Yemen, Palestine, and Syria gain experience from larger centers. However, virtual meetings may reduce engagement compared with in-person peer reviews.
This study provides valuable insights but has limitations. First, the cross-sectional nature of the survey limits the ability to establish causal relationships between variables. In addition, self-reported data may introduce biases, affecting accuracy and reliability of the findings. Despite being adapted from previous studies and piloted for relevance, the survey might not capture nuances of peer review practices in various cultural and institutional contexts within the MENAT region.
In conclusion, this study sheds light on the current status of radiation oncology peer review in the MENAT region. Despite numerous obstacles and challenges to implementation, it is still highly valued, both as an opportunity for education and for enhancing patient care. It is widely implemented in most centers in the region, especially in those with more advanced technologies and techniques. However, region-specific guidelines should be placed to enhance and sustain these vital practices.






