Mount Lebanon Hospital’s Diabetes and Obesity center, established in June 2007, offers to patients a multidisciplinary approach to diabetes and their health. Staffed by highly-qualified Endocrinologists, a diabetes nurse educator (DNE) and a dietitian, there is no doubt that every patient will have all their medical issues addressed during visits to this Center. People with diabetes need ongoing care in a patient centered, supportive, and positive environment, without barriers to obtaining care.
Aiming to provide medical care to all patients, Mount Lebanon Hospital and its Diabetes and Obesity Center work together on strategic plans to increase the level of awareness of the morbidities related to obesity, hypertension and diabetes.
Patients will learn about their disease, its complications, management and how to overcome its burden. Along with lifestyle modification by diet counseling and exercise.
Mount Lebanon Hospital Diabetes & Obesity Center works hand in hand with other medical specialists in the Hospital such as Nephrologists, Cardiologists, Ophthalmologists, Orthopedic, and Vascular surgeons and many other healthcare professionals, to insure high standards of care and up-to-date technologies and knowledge for all patients.
Overview
Diabetes occurs when the body does not properly process food as energy. When patients have diabetes, their body either does not respond to insulin or does not produce any.
Insulin is a critical hormone that transfers glucose to the cells in the body, causing sugars to build up in blood, which puts patients at risk of serious complications.
Types of Diabetes
- Type 1 Diabetes:
- Develops among children or young adults;
- The body produces very little or no insulin;
- Type 1 patients:
- Resolve to daily insulin injections to control glucose levels;
- Need constant lifestyle monitoring.
- Type 2 Diabetes:
- Can occur at any age;
- Insulin resistance and deficiency;
- Type 2 patients:
- Can manage their condition through exercise and diet;
- Most people, over time, will require oral drugs intake and/or insulin injections.
- Gestational Diabetes Mellitus (GDM):
Any woman can develop gestational diabetes during pregnancy! This type of diabetes can affect the health of the mother and her baby. Some women are more at risk

Any pregnant woman is at risk of developing gestational diabetes during the second or third trimester. Here are different methods to prevent or treat it:
– Consult a dietitian to set up a diet plan
– Engage in physical activity, after getting medical clearance
– Monitor blood sugar level regularly
– Follow physicians’ recommendations, including insulin treatments when required
When blood glucose levels are not controlled, gestational diabetes can cause:
– C-section
– Excessive birth weight
– Low blood sugar (hypoglycemia)

- A hormone made by the placenta prevents the body from using insulin effectively;
- Glucose builds up in the blood instead of being absorbed by the cells;
- Referred to as insulin resistance;
- Gestational diabetic symptoms disappear after delivery;
- Treatment may include:
- Special diet;
- Exercise;
- Daily blood glucose monitoring;
- Insulin injections.
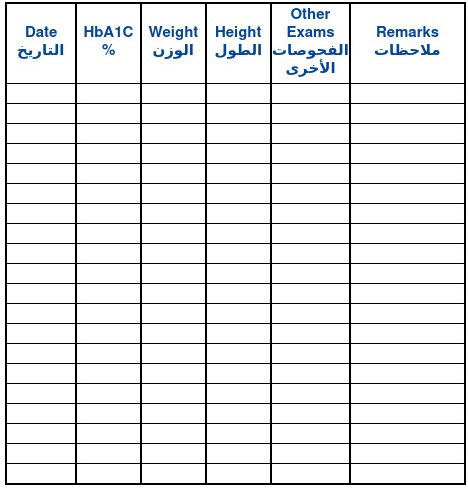
Ranges of Blood Glucose

Diabetes can slow you down, it can make your life different but it does not have to stop you with Ramadan. Read the article on the link in the bio for tips on how to manage your diabetes this Ramadan.
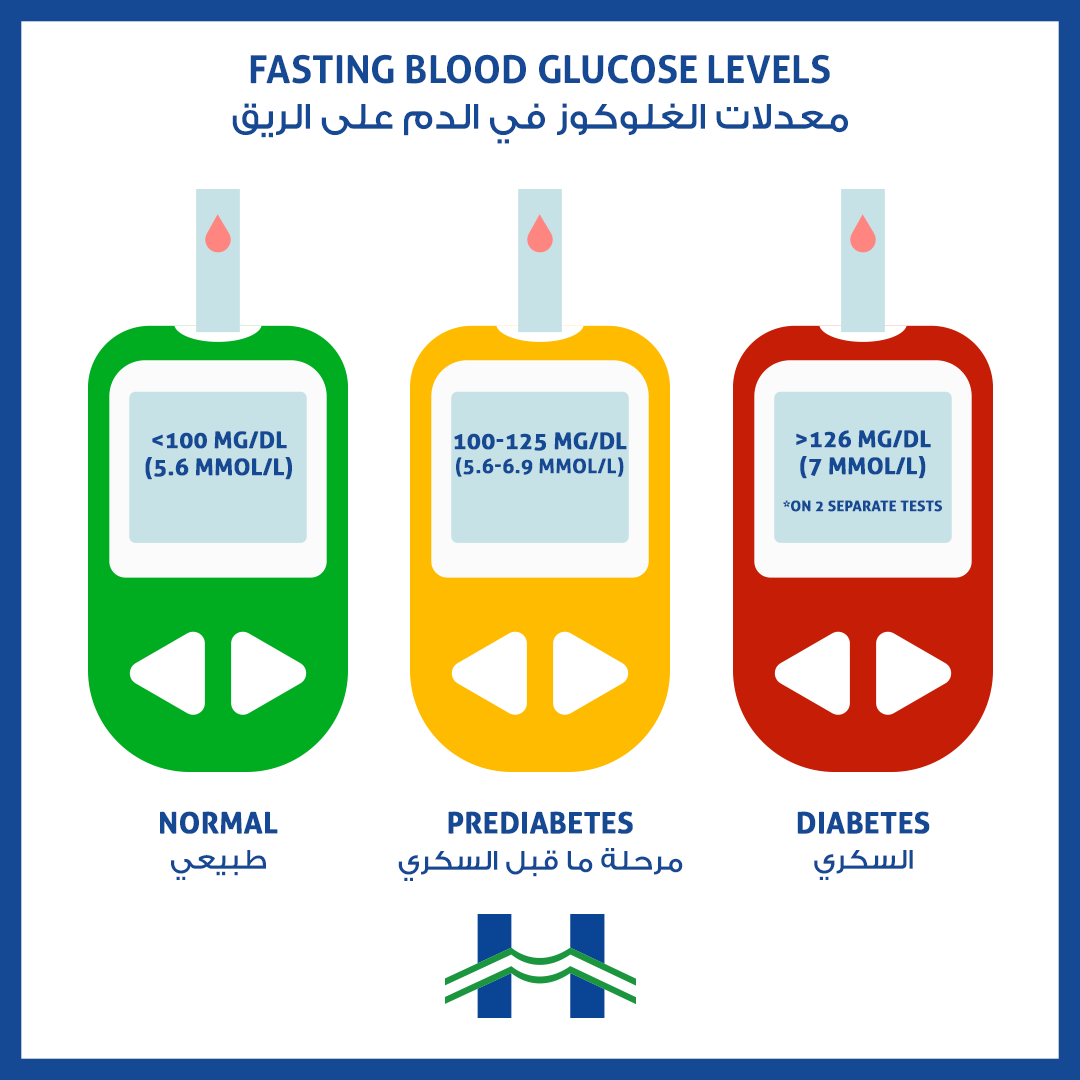
Know the sufficient insulin numbers!
For more information, visit our endocrinologist at the Mount Lebanon Hospital Diabetes Center for guidance or call 71 998822
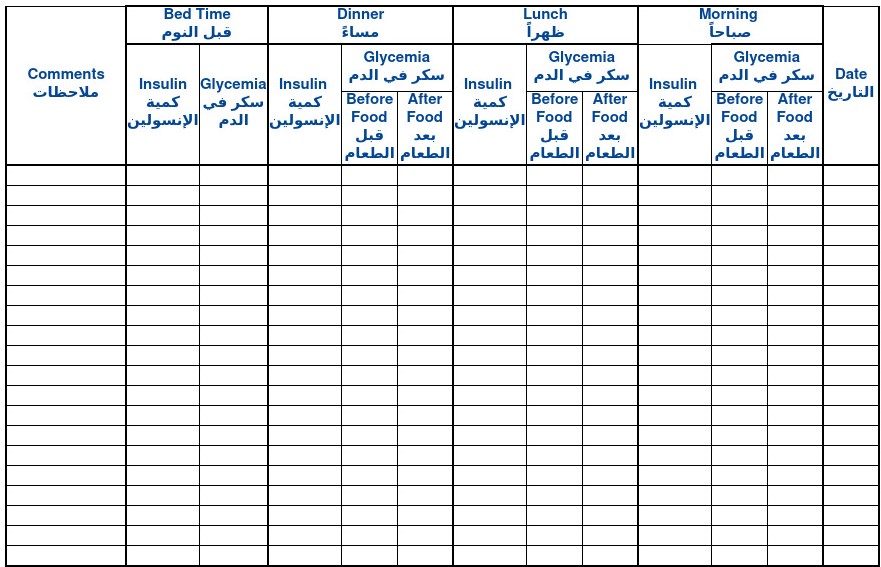
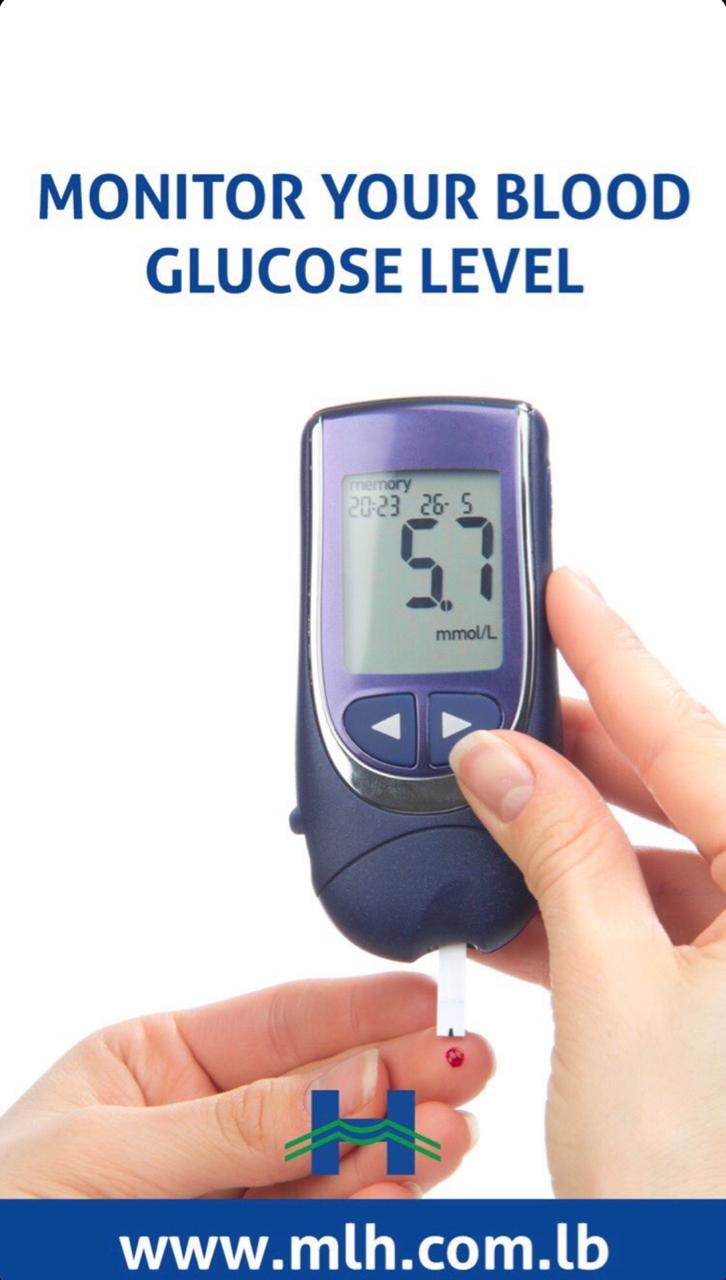
Blood glucose testing is usually recommended before meals and at bedtime. The most known method is finger-stick checks, where patients pick the tip of their finger with a small needle, put a drop of blood on a testing strip then insert it into a meter, fifteen seconds later the results will appear on the screen.
Blood glucose testing is usually recommended before meals and at bedtime. The most known method is finger-stick checks, where patients pick the tip of their finger with a small needle, put a drop of blood on a testing strip then insert it into a meter, fifteen seconds later the results will appear on the screen.
The newest type of continuous glucose monitor is an implanted sensor under the skin that can detect blood sugar levels for up to three months. The transmitter sends blood sugar information wirelessly from the sensor to a beeper or a smartphone app.
Patients should consult with their physician concerning the types of monitoring required for their case. Any values higher or lower than the flowing normal ranges must be consulted immediately by a physician.
Non-diabetic Normal blood glucose ranges:
- Before meals: 70-99 mg/dl;
- 2 hours after a meal: <140 mg/dl;
Target blood glucose ranges for diabetic patients:
- Before meals: 70-130 mg/dl;
- 2 hours after a meal: <180 mg/dl;
HbA1C Normal ranges:
- Non-diabetic: < 5.7%
- Diabetic: < 7%
HbA1C blood test must be repeated every 3 months, or as prescribed by the physician.
Symptoms of Diabetes







You should consult a doctor if any of the following warning signs is suspected:
- Frequent urination during the day and night;
- Increased thirst;
- Hunger and need to eat sugar;
- Extreme fatigue;
- Blurred vision;
- Slow healing wounds;
- Unexplained weight loss;
- Tingling, pain, or numbness in the hands and/or feet.
Complications of Diabetes
Over time, the effects of diabetes can cause severe complications. Without treatment, the disease can lead to serious, even life-threatening conditions. Early detection is key; therefore diabetic patients should consult with a multidisciplinary team of physicians to prevent complications from escalating.
These conditions range from macro vascular to micro vascular diseases:
Micro vascular diseases
a. Diabetic Retinopathy (Eye injury)
A leading cause of visual disability, caused by small blood vessel damage to the back layer of the eye, the retina. It leads to progressive loss of vision, even blindness. This can be diagnosed through regular eye examinations.
b. Diabetic Nephropathy (Kidney disease)
Also known as deterioration of kidney function, diabetes causes damages to small blood vessels in the kidneys, may lead to kidney failure. In developed countries, diabetic nephropathy is a leading cause of dialysis and kidney transplant. Patients can be diagnosed by a urine test and a blood test.
c. Diabetic Neuropathy (Nerve disease)
Nerve damage occurs among diabetic patients suffering from hyperglycemia, direct small blood vessels damage caused by hyperglycemia (high blood sugar levels) and decreased blood flow. Nerve damage can lead to sensory loss, limbs impairment and weakness among diabetic patients, and can be diagnosed through a physical exam and blood tests.
Keep feet healthy with Diabetes!
d. Cardiovascular disease
High blood sugar (hyperglycemia) damages blood vessels through a process called “atherosclerosis” or arteries clogging. This narrowing of arteries can lead to decreased blood flow to the heart muscle (causes a heart attack), or to the brain (leads to a stroke), or to extremities (leads to pain and reduces infections healing). Early detection can delay progression, primary prevention includes smoking secession, high blood pressure control, high cholesterol and obesity treatment. This can be detected by blood tests, echocardiography, stress testing and cardiac MRI.

In some cases, obesity is caused by the over-production of the cortisol hormone due to corticosteroids intake or hormonal imbalance. This is manifested as the Cushing’s syndrome, hence it is recommended to consult an endocrinologist.

Did you know that people suffering from diabetes are 2 to 4 times more likely to develop heart disease? This is caused by the following reasons:
– Higher blood pressure
– Higher cholesterol, triglycerides and glucose levels
– Higher level of obesity and lower physical activity
Take action today to protect yourself against heart disease!
Hyperglycemia
Hyperglycemia refers to high blood sugar levels, mostly affects diabetic patients.
a. Signs and symptoms of Hyperglycemia
Symptoms of hyperglycemia develop slowly over several days or weeks. The longer blood sugar levels stay high, the more serious the symptoms become.
Early signs and symptoms:
- Frequent urination;
- Increased thirst;
- Blurred vision;
- Fatigue;
- Headache.
Later signs and symptoms:
- Fruity-smelling breath;
- Nausea and vomiting;
- Shortness of breath;
- Dry mouth;
- Weakness;
- Confusion;
- Abdominal pain;
- Diabetic coma.
b. Causes of hypoglycemia
Many factors can contribute to hyperglycemia among diabetic patients, including:
- Lack of insulin / oral diabetes medication intake;
- Incorrect injection of insulin;
- Disrespect of recommended eating plan;
- Inactive lifestyle;
- Use of expired insulin;
- Illness or infection;
- Certain medications (i.e. steroids);
- Injury;
- Surgery;
- Emotional stress (family conflict, workplace challenges, etc…).
c. Hyperglycemia treatment
If left untreated, hyperglycemia can become severe and lead to serious complications requiring emergency care, such as a diabetic coma. Patients should consult with their diabetes management team concerning treatment options, mostly treatment includes:
- Regular exercises;
- Proper medication and insulin intake;
- Food consumption management;
- Regular blood sugar monitoring.
Hypoglycemia
Hypoglycemia refers to low levels of sugar, or glucose, in the blood (less than 70mg/dl). It is not considered as a disease, but it can indicate a health problem. Hypoglycemia can occur due to several conditions, but it is most commonly a reaction to medications, such as insulin; therefore diabetic patients should consult with their care team concerning their blood glucose target and the levels that are considered too low for their case.
a. Signs and symptoms of hypoglycemia
Every individual’s response to low blood glucose level is different. Most common signs and symptoms are:
- Shiver and tremble;
- Sweat and chills;
- Irritability or impatience;
- Nervousness or anxiousness;
- Confusion;
- Fast heart beat (palpitations);
- Dizziness;
- Hunger;
- Nausea;
- Blurred/impaired vision;
- Tingling or numbness in the lips, tongue or cheeks;
- Headache.
b. Causes of Hypoglycemia
Risk factors of hypoglycemia happens when patients:
- Skip or delay a meal or a snack;
- Increased dosage of insulin;
- Low carbohydrates intake;
- Exercise;
- Consume alcohol, especially without eating carbohydrates.
c. Treatment of Hypoglycemia
- 3-4 glucose tablets; (prescribed by the physician)
- 4-6 pieces of hard candy (avoid sugar-free);
- ½ cup fruit juice;
- 1 cup of skimmed milk;
- ½ cup of soft drink (avoid sugar free drinks);
Monitor glucose every 15 minutes and consult a physician for advice.
Diabetes Prevention

In 2016, the WHO released facts about diabetes prevalence in Lebanon:
– 4% of mortalities in Lebanon are caused by diabetes – 12.6% of the upper middle income section of the population suffers from diabetes
– Men have a higher prevalence of developing diabetes compared to women
Find out more at the Diabetes & Obesity Center at MLH… serving you since 2007
Type 1 diabetes: is not preventable, it involves an inherited susceptibility to developing the disease, if a family member has or had type 1 diabetes one is at a higher risk; If both parents have or had type 1 diabetes, the likelihood of their child developing this disease is higher than one deceased parent.
Type 2 diabetes: there are a number of factors that can influence its development, such as unhealthy food consumption and inactive lifestyles. Studies from different parts of the world have established that lifestyle modification with physical activity and/or a healthy diet can delay or prevent type 2 diabetes onset.
Diabetes Management




Diabetes is not curable, but it can be controlled through:
- Diet and exercise only;
- Diet and exercise, oral medications and blood glucose self-monitoring;
- Diet and exercise, insulin therapy and blood glucose self-monitoring;
- Use a pedometer to keep count of your movements throughout the day.
Dr. Marie Feghaly Merheb, Endocrinologist at Mount Lebanon Hospital explains the role of family in the management and support of #diabetes
Diet Management

Artificial sweeteners simulate the sweet taste of sugar with less calories. They are also called sugar substitutes and are considered helpful in fighting obesity, diabetes and metabolic syndrome. These conditions are considered dangerous since they present a risk factor for heart diseases. Therefore, the American Diabetes Association and the American Heart Association recommend artificial sweeteners to a certain extent
Diabetes: A guide to dining out

Diabetic patients’ simple diet management guide:
- Plan meal times and avoid skipping meals during the day;
- Eat small and frequent meals;
- Maintain a varied and balanced diet;
- Distribute complex carbohydrates intake evenly between meals;
- Add a fruit after each main meal;
- Increase fiber intake;
- Eat less fat or oil;
- Exercise regularly, make it a daily routine (find a partner to exercise with);
- Avoid alcohol intake;
- Choose fresh vegetables, fruits and whole grain bread;
- Consume non-starchy vegetables.
General Tips
Diabetes, whether it is type 1 or 2, should not stop you from travelling. Here are some tips to help you pack for your trip:
1- Get a prescription letter from your doctor describing your medicine and prescription.
2- Pack at least twice as much medication and blood-testing supplies as you think you need.
3- Pack all of them in your carry-on bag so that your medication is always with you
Live well with diabetes and make sure to:
- Get regular check-ups:
- Check blood glucose at least twice per day;
- Undergo HbA1C test every 3 months;
- Control blood pressure, cholesterol and triglycerides levels;
- Regular clinic visits for physician’s consultation.
- Track carbohydrates intake;
- Lose extra weight and follow a healthy diet;
- Maintain an active lifestyle;
- Take medications as prescribed by the physician;
- Manage stress;
- Make sure to memorize the insulin name (if applicable);
- Get enough sleep;
- Check feet every day for cuts, blisters, red spots and swelling;
- If diabetic and planning to get pregnant it is important to consult the physician before conceiving.